The long-awaited scoping study has finally been published. This document defines “high-burden under-researched medical conditions” that will be targeted in future calls of the Horizon Europe research program. ME/CFS made the list but so did a lot of other medical conditions. This article provides a brief overview of the main results.

Background and introduction
The scoping study was ordered by the European Commission. Partly instigated by the ME/CFS resolution, the Commission wanted to better define a group of medical conditions that have a high disease burden but have thus far been under-researched. The idea was that these conditions could then be targeted in future calls of the Horizon Europe research program to reduce inequities in research funding.
The scoping study was conducted by an independent team of Dutch researchers at NIVEL, the Institute for Health Services Research in the Netherlands. Their report was published on 18 January 2023.
The methodology used
The authors used 4 different methods to identify under-researched medical conditions.
- First, they examined the amount of past EU research funding per group of medical conditions as defined by the International Classification of Diseases version 11 (ICD-11). The five groups of medical conditions that received the least EU funding were selected
- Second, they looked at parameters collected by the Global Burden of Disease (GBD) study and compared these to the amount of EU research funding received. The burden metrics used were prevalence, disability-adjusted life years (DALYs), years of life lost (YLL), and mortality. The 10 most underfunded conditions for each disease burden metric were selected.
- Third, the authors looked at papers that describe medical conditions for which people visit their general practitioner (GP). The NIVEL researchers hoped that this would help identify common but high-burden conditions that were overlooked by the first two approaches.
- Fourth, stakeholders were asked to provide feedback to a temporary list and add any additional high-burden under-researched medical conditions. Stakeholders included patients and citizens, healthcare professionals but also EU Member State representatives, members of academia, and public funding bodies. EMEC and our colleagues at the World ME Alliance were able to provide feedback as stakeholders.
Conditions were excluded from the final list if it concerned a rare disease, there was no evident knowledge gap concerning etiology and treatment for the condition, or the funding received was already high. For example, cardiovascular diseases and cancers were identified by the second approach but these conditions were excluded because they already receive large funding amounts and have research programs dedicated to them. Other conditions such as caries or chronic obstructive pulmonary disease (COPD) receive little research funding compared to their prevalence but were excluded because there is no clear knowledge gap. Both the etiology and treatment of these conditions are already known.
Which diseases made the final list?
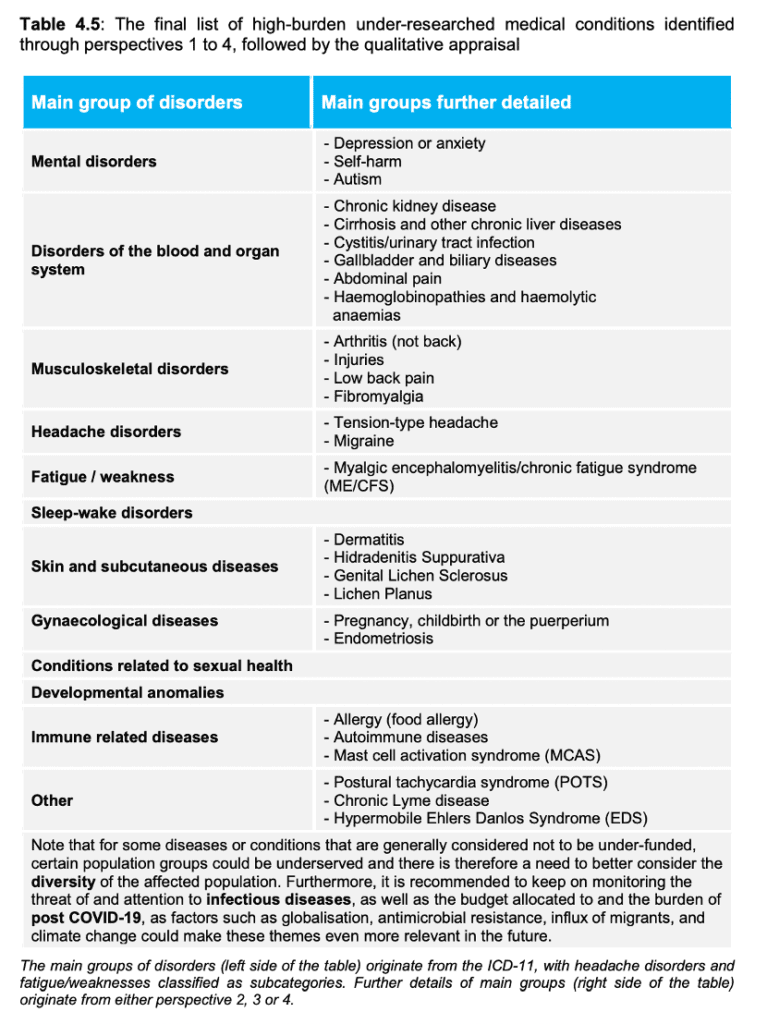
The diseases that made the final list of high-burden under-researched medical conditions are shown in table 4.5 on page 18 of the report.
Let’s have a closer look at the list and the methods that created it.
The first approach identified large groups of medical conditions such as pregnancy and childbirth, sleep-wake disorders, or conditions related to sexual health. This method looked at chapter averages of the ICD-11. It focused on illness classifications and was largely dependent on how the ICD categorizes conditions. If an under-researched illness is clustered inside a large group of diseases that are not underfunded, it would easily be overlooked by this approach. This seems to have happened with ME and CFS which are both housed under ‘Disease of the Nervous System’ in the ICD-11.
The second approach identified conditions such as low back pain, chronic kidney disease, migraine, and mental disorders. The limitation of this method, however, is that the GBD study did not estimate the disease burden of all illnesses. There is no GBD estimate for ME/CFS, for example, which means the illness could not be identified by this approach. EMEC has been in contact with GBD researchers to include ME/CFS in future disease burden estimates. A concrete research project proposal was on the table but unfortunately, we were unable to find funding for it. Ironically, research on ME/CFS is so underfunded that it is unable to provide a GBD estimate.
The third approach resulted in a list of conditions for which people visit their GP. These included abdominal pain, back pain but also dermatitis, hypertension, and arthritis. Fatigue/weakness was mentioned but not ME/CFS. A likely explanation is that ME/CFS often remains undiagnosed and is not easily identified by GPs. If a diagnosis is made, it is usually done by ME/CFS clinics or specialists in internal medicine.
Most of the illnesses that we regard as under-researched relative to disease burden were identified by the fourth approach that queried stakeholders. These include ME/CFS but also Hypermobile Ehlers-Danlos Syndrome (hEDS), Postural tachycardia syndrome (POTS), fibromyalgia, endometriosis, chronic Lyme disease, and Long Covid. 44 Out of 130 stakeholders contacted, responded to the NIVEL survey, a response rate of only 20%. The risk of selection bias is therefore the main limitation of this approach. Some stakeholder groups might have been overrepresented or underrepresented.
How to move forward
The authors of the report highlight many limitations of their study and indicate that this is only a first attempt at identifying under-researched conditions.
We believe that their reliance on existing databases and classification systems resulted in a rather long and heterogenous list. The conditions that are most underfunded do not yet have GBD estimates or an obvious classification inside the ICD-11. They are often not recognized or diagnosed in primary care. This is certainly the case for ME/CFS.
The group of diseases on the final list is quite heterogeneous. Some of the medical conditions listed such as pregnancy or injuries are not considered a disease. Others are already included in established disease categories that are frequently the target of funding opportunities and calls for applications. Depression and anxiety, for example, fall under mental health conditions, low back pain and headache under pain conditions, dermatitis under skin conditions, etc. While it may be true that many of these are underfunded, they already have a “home” in an established classification. It might therefore make more sense to address their lack of recognition and funding inside these existing categories.
If you subtract the medical conditions mentioned above, a group of “homeless” neglected diseases becomes visible. These are illnesses that are prevalent and disabling but poorly understood. Consequently, it is not yet clear to which category they belong. Little is known about their pathology, so they often remain undiagnosed. We believe it would be valuable to make this a new, separate category that could be targeted in EU research programs.